Diabetes and Depression: A Toxic Combo for Suicide
Diabetes and Suicide
Suicide is a serious problem.
Depression, especially when combined with other disorders and illnesses, can make you feel like it is not making any headlines.
Depression and Diabetes: A Toxic Combo for Suicide
Heart and kidney failure, and limb amputation, are all occurrences that are non-diabetics that do not have to deal with. It can be very frustrating and depressing- especially if you do not know many other people who can empathize or relate.
Susan Guzman, Ph.D., director of clinical services for the Diabetes Behavioral Institute in San Diego, says “Mortality rates in people who have both diabetes and depression are about 2.5 times the rates.”
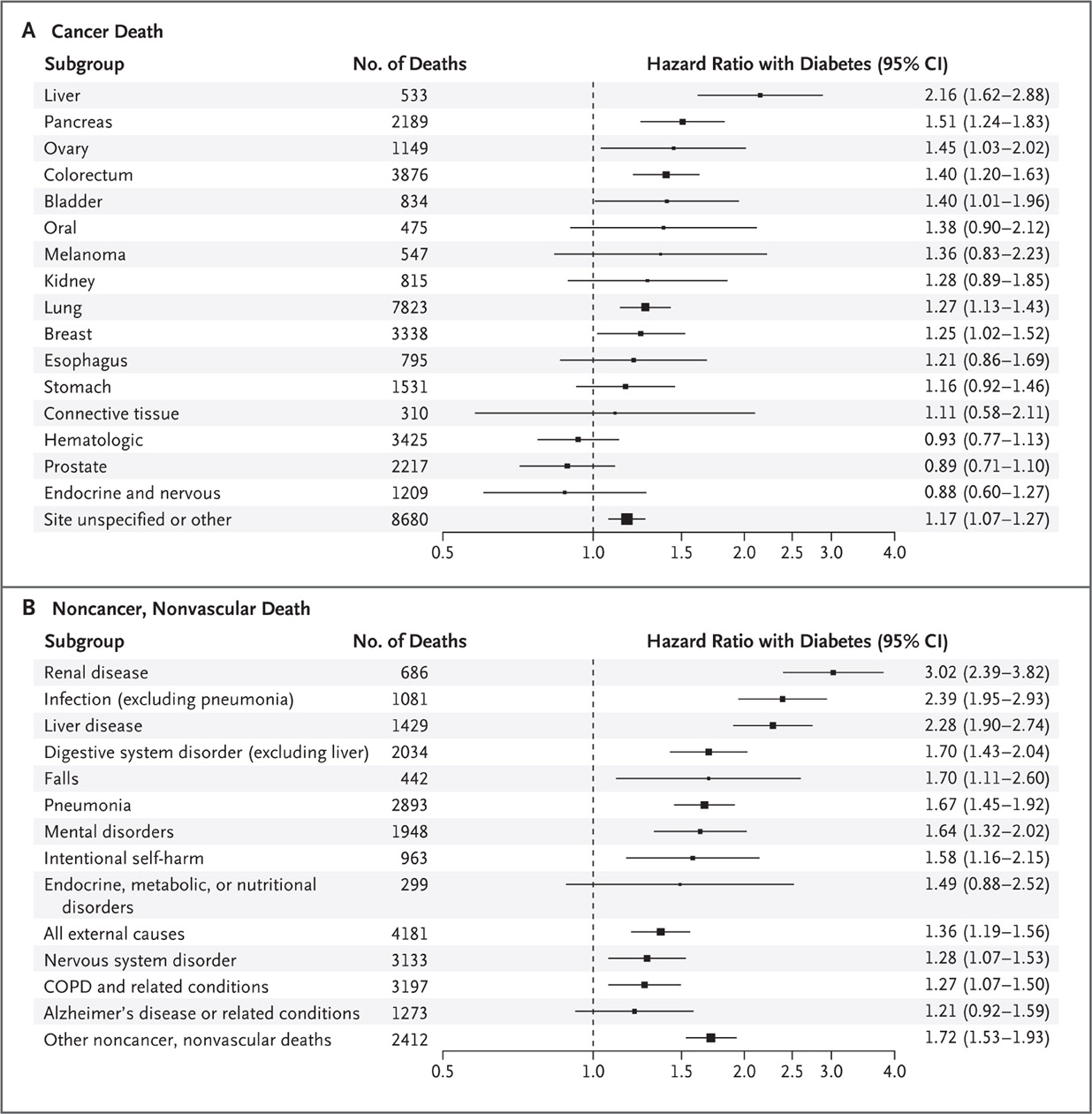
Intentional self harm Resulting in death or suicide, has a higher hazard ratio than Neurological disorders, Alzheimer’s, and COPD-related deaths among diabetics as you will see in the table below in section B. That Means a diabetic is more likely to commit suicide than the from mental or neurological disorders .
That is terribly unsettling.
Another study went as far as saying diabetics were 58 percent more likely to die from suicide , mostly Because theywere more likely to be depressed. Indeed, it has been shown to cause chronic stress and strain, which in the long run, may increase the risk of depression.
The combination of diabetes and depression compliment each other in the worst way possible at times. Coexisting depression in people with diabetes is associated with decreased adherence to treatment, poorer metabolic control, higher complication rates, decreased quality of life, increased healthcare use and cost, and increased risk of death.
Suicide by Insulin
A common method of suicide attempt in patients with diabetes includes uses of high doses of insulin or other medications to treat the disease.

How You Can Help: Tips for Preventing Diabetic Suicide
Know the Signs of Diabetic Depression
Depression leading to intentional self harm usually doesn’t just appear out of thin air. Often signs are ignored and cast aside as if not important or real. “Look for any kind of warning signs,” says family medicine expert David Katerndahl, MD, and take action. “Don’t sit on it. You’re better off talking to the patient or the physician and, if it turns out your wrong, that’s fine. You don’t want to end up second-guessing yourself.” Your awareness and insistence could make the difference in you or your loved one’s life.
Two-thirds of doctors fail to recognize depression.
It may be because they didn’t ask or the patient didn’t tell. Either way, you can play a vital role in spotting these signs:

4 Major Signs of Diabetic Burnout
Diabetic burnout is a type of psychiatric morbidity resulting in a genuine disregard for managing diabetes and can lead to depression but can also be caused by depression which puts diabetics at great health risks including self harm and long-term complications like limb amputations, diabetic blindness (retinopathy), and organ failure.
Diabetic burnout usually happens due to the complex nature of managing diabetes and stress associated with the disease. Diabetics know that no two days are the same and no matter how tight your blood sugar control and general management is, there will be anomalies and variables that occur. The lack of control in diabetes tends to be one of the most frustrating parts.
The 4 major signs of diabetic burn out are:
- Negligence about medical care. This is one of the most dangerous signs of diabetes burnout. Cancelling doctor’s appointments, not taking medications as prescribed, eating poorly, not checking blood sugars and not exercising are warning signs that you’re not taking care of yourself as you should.
- Social withdrawal: Distancing yourself from family, friends, doctors etc can be a signal of depression and diabetic burnout
- Decline in activity or performance level: Reaching a point of just getting by or doing no more than the minimum that is physically or mentally required of you may suggest diabetes burnout.
- Emotional exhaustion: Managing a chronic illness like diabetes takes an emotional toll and can leave you feeling exhausted, overwhelmed, and down.
Emotional Support for Diabetic Depression
Accepting your feelings is the first step. It’s okay to feel frustrated, angry, or sad so don’t hold back your feelings. Reach out to trusted friends and family. Find a diabetes support group where you can talk with others who can relate to what you’re facing.
Thankfully, with social media today, support is endless. I only know of one other type 1 diabetic my age in my area but with Facebook groups like Daniel Borba’s Type 1 Athletes and meet ups, I am in contact and supported by thousands of others going through the same struggle. The emotional support is 1 click away in most cases and I have life long friends because of it so I highly encourage people with diabetes to do a search on Facebook for type 1 diabetes groups and connect with others.
Along with social media, many areas have group meet ups for diabetics. You can ask your endo, google local type 1 diabetes groups, or checkout meetup.com for local events.
Medical Support for Diabetic Depression
If you are struggling with depression or know someone who is, talk with your doctor. Ask for a referral to a mental health professional. Research indicates that professional counseling, sometimes in combination with anti-depressant medication, is a very effective treatment for depression. Regular screening for suicidal ideas and appropriate psychiatric management of the symptoms can help in reducing potentially fatal outcomes.
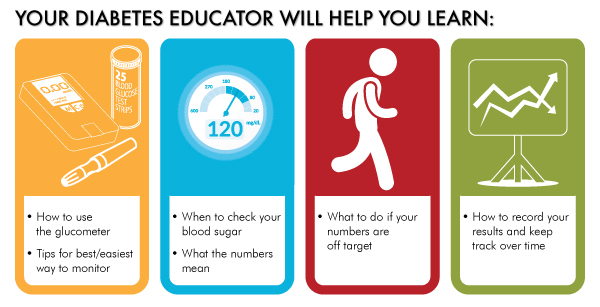
Talk to your endocrinologist. Seek a local CDE (certified diabetes educator) in your area or work with one remotely via Skype like Gary Sheiner or Kelley Crumpler.
Ed Cook, a San Diego resident, was diagnosed with diabetes 38 years ago. For much of the time, the government administrator and, after retirement, entrepreneur felt life was balanced despite his illness. But as Cook, now 66, gradually lost his vision and then his driver’s license, his business, and most recently, one toe to amputation, depression infiltrated his life.
“The complications led me to severe depression,” Cook admitted. He tried anti-depressants for a time, and now regularly attends both therapy and support groups. “It helps to know I am not alone,” he said. “Diabetes is not the end of the world. Getting treated for depression was a godsend,” said Cook.
Setting Goals
On top of emotional support, group therapy, and professional medical help, setting new goals and actively engaging in hobbies can also help with diabetes and depression management. Personally, I vouch for how fitness saved my life (read more about my story On Beyond Type 1’s website here).
I help type 1 diabetics lose weight, get stronger, and most importantly, improve their confidence with my online fitness and nutrition coaching. I know what it is like to be in a dark place in your life. Getting in the gym and improving my body not only helped my diabetes management but provided me with a way to overcome depression. It’s really hard to be negative when you see positive changes in your body.
References
- Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM: Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 23: 434–442, 2000
- Agnieszka Butwicka, Louise Frisén, Catarina Almvqvist, Björn Zethelius, Paul Lichtenstein: Risks of Psychiatric Disorders and Suicide Attempts in Children and Adolescents With Type 1 Diabetes: A Population-Based Cohort Study. Diabetes Care 2015 Jan; dc140262.
- Lustman PJ, Griffith LS, Clouse RE, Freedland KE, Eisen SA, Rubin EH, Carney RM, McGill JB: Effects of nortriptyline on depression and glucose regulation in diabetes: results of a double-blind, placebo-controlled trial. Psychos Med 59:241–250, 1997
- Lustman PJ, Griffith LS, Freedland KE, Kissel SS, Clouse RE: Cognitive behavior therapy for depression in type 2 diabetes: a randomized controlled trial. Ann Intern Med 129:613–621, 1998
- Lustman PJ, Freedland KE, Griffith LS, Clouse RE: Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care 23: 618-623, 2000
- Darok M, Gatternig R. Suspected suicide and suicide attempt with mysterious concomitant circumstances. Forensic Sci Int. 2005; 147 (Suppl): S17-9.
- Jacobson AM, de Groot M, Samson JA: The Effects of Psychiatric Disorders and Symptoms on Type II Diabetes Mellitus. Qual Life Res 6: 11-20, 1997
- Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care2008; 31: 2383-239

